Butonitazene and Isotonitazene
Butonitazene and Isotonitazene are synthetic opioids first synthesized in the 1950s and are AS potent as fentanyl. Isotonitazene has recently begun to appear in the lab results of individuals who have suffered fatal overdoses. In a case control study reported in the journal American Society of Addiction Medicine, in a six-month period in 2020, there were 40 fatal overdoses involving Isotonitazene in Cook County, Illinois and Milwaukee County, Wisconsin. Isotonitazene is often mixed with cocaine or other drugs, making it more lethal. Butonitazene has not yet become the problem that Isotonitazene has, but it is readily available online through multiple outlets. As with other opioids, ingesting either Butonitazene or Isotonitazene can cause respiratory depression, rapid or declining heart rate, loss of consciousness, vomiting, and hallucinations or delusions, as well as death.Etizolam
Etizolam has been called a “new alternative” to Xanax. It is related to benzodiazepines and is used as a prescription medication in Japan, Italy, and India to treat anxiety and sleep disorders. It is NOT, however, approved for any medical use in the United States. Here in the United States, it is treated by law enforcement as a recreational substance. Etizolam ingestion can cause hallucinations, agitation, and a high risk of overdose. Because it is not an opioid, Narcan or Naloxone is ineffective when encountering a person experiencing an Etizolam overdose.Grey Death and Smurf Dope
Grey death and Smurf dope are dangerous drugs that are becoming prevalent in a number of states across the country. They contain a combination of methamphetamine or heroin and fentanyl and/or carfentanil, a Fentanyl analog. Grey death, so named because it resembles concrete, is described as being so deadly that merely touching it can result in death, with a potency 10,000 times greater than morphine. Smurf dope is a vibrant blue drug that has been linked to a rash of fatal and nonfatal overdoses in Kentucky. A pattern of regional emergence with these lesser-known substances that then spreads to a wider geographical influence is typical with newer substances of abuse. Because fentanyl and carfentanil are opioids, a person experiencing an overdose on Grey Death or Smurf Dope can be treated with an opioid overdose reversal drug such as Naloxone.Khat
Khat is a plant-based stimulant drug found in Africa that has been effectively listed as a Schedule I substance in the United States since 1993. However, in recent months, more than 1,000 pounds of Khat has been seized in two U.S. cities, signaling that Khat abuse might be on the rise. The effects of Khat are very much like cocaine and other amphetamines. High doses of Khat can result in delusions, violence, hallucinations, and schizophrenic psychosis.Lean
Made famous by musicians around the globe, lean, or “sizzurp,” “purple drank,” or “water,” is a mixture of cough syrup with codeine, soda, and hard candy. It is most popular with young adults and teens. Because codeine is an opioid, although not as strong as heroin or fentanyl, it is addictive and can be abused or cause death.Tianeptine/Tianaa
Tianeptine is an antidepressant drug approved for use to treat anxiety and depression in many European, Asian, and Latin American countries, though NOT approved for use by the U.S. Food and Drug Administration. It can be found being sold online as a dietary supplement or a so-called “research chemical,” which is a term typically used by online sellers/dealers to describe NPS for sale to make the substances seem legitimate. It has been categorized as a Schedule II controlled substance in a few states. Tianeptine is the main ingredient in Tianaa, a drug marketed as an herbal supplement and sold in gas stations and other convenience stores, but which is potentially very dangerous and addictive. According to the Drug Enforcement Administration, tianeptine use can result in severe withdrawal symptoms resulting in hospitalization as well as respiratory, neurological, cardiovascular, and gastrointestinal effects. Poison control center calls related to exposure to tianeptine increased an incredible 1,700 percent during a 3-year span alone. There is some evidence that a tianeptine-related overdose can be reversed through the administration of an opioid overdose reversal drug such as naloxone.Purple Heroin
Purple heroin is a mixture of a number of drugs, including heroin, oxycontin, acetaminophen, fentanyl or carfentanil, and a new drug called brorphine which is a synthetic opioid. The substance is purple in color, and individuals who overdose on it may experience blue nails and lips, confusion or lethargy, snoring or choking sounds, difficulty staying alert, and weakened or absent breathing. As with other opioid-related overdoses, naloxone may help someone experiencing an overdose on purple heroin.Xylazine
Better known as “tranq,” xylazine is a non-opioid sedative used by veterinarians as a tranquilizer. It is often combined with an opioid to create what is known as “tranq dope.” It first appeared regionally in Puerto Rico in the early 2000s but has since been increasingly seen in overdose deaths throughout the mainland. Overdoses in Connecticut involving xylazine doubled from 70 deaths in 2019, when the drug first appeared, to 140 deaths in 2020, and that number is increasing in other locations. In Philadelphia, for example, the percentage of overdose deaths where xylazine was present increased to 31 percent, up from a low of just two percent between 2010 to 2015. Because xylazine is not an opioid, treatment with an opioid overdose reversal drug such as naloxone is ineffective.Conclusion
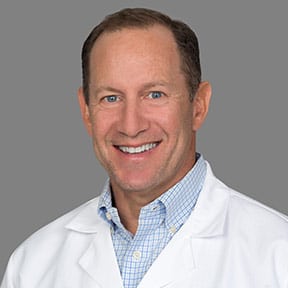
Dr. Kenneth Spielvogel is a board-certified Physician with a focused interest in addiction medicine. He is dedicated to providing comprehensive and compassionate care to patients throughout all stages of life. With nearly 30 years of experience, he combines his expertise with a genuine warmth and attentiveness, making him a trusted choice for patients seeking personalized healthcare. From Inspiration to Dedication: Inspired by his father’s career in medicine, Dr. Spielvogel followed his own path, choosing to specialize initially on women’s health. Seeing the devastation of drug and alcohol use disorders on his patients, he focused his continuing education on all aspects of addiction medicine. He continues to integrate this knowledge into both inpatient and ambulatory care.
Areas of Expertise:
Dr. Spielvogel offers a wide range of services, including:
- Menopause and hormone replacement therapy (HRT)
- Family planning and infertility
- Abnormal bleeding disorders
- Minimally invasive surgery and robotics
- Preconception counseling and prenatal care
- Annual exams and preventative care
Full scope treatment of addiction and recovery A Personalized Approach:
Dr. Spielvogel believes in building strong relationships with his patients. He takes the time to understand their individual needs and concerns, tailoring his approach to ensure they feel heard and supported. He also speaks fluent Spanish, enabling him to serve a diverse community. Beyond the Exam Room: Dr. Spielvogel is passionate about empowering patients to make informed decisions about their health. He enjoys counseling patients on healthy lifestyle choices, including weight management, and stays up-to-date on the latest advancements in all aspects of healthcare.
Education and Affiliations:
- Medical Degree: George Washington University School of Medicine
- Residency: University of Colorado Health Sciences Center
- Board Certification: American Board of Obstetrics & Gynecology
Affiliations:
MemorialCare Medical Group Long Beach, Pediatrix Medical Group Consultant and clinical care member for both One Method and Carrara treatment centers